Melasma refers to a chronic, recurrent, symmetrical brownish discoloration affecting predominantly the curvatures of the face. The shoulders and upper arms are less commonly affected. It is also referred to as Chloasma or “the mask of pregnancy” when it affects pregnant women. Melasma originates from the Greek word for black while Chloasma has its origins in reference to the Greek for green.
This condition predominantly affects women and is seen between the ages of 20-40 yrs in all races. Individuals who tan well and have darker skin seem to be more susceptible but some families are affected more than others.
The exact cause is not known but there is an overproduction of melanin by the pigment cells (melanocytes) which results in pigment being found near the surface (epidermis) and/or deeper in the skin (dermis).
The most important risk factor for Melasma is sun exposure and its associated ultra violet damage to the skin. This is totally avoidable but more likely and prevalent in locations close to the equator. Hormonal contributions from pregnancy and contraception also play an important part. Hypothyroidism is also an uncommon association with the condition.
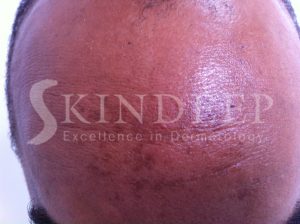
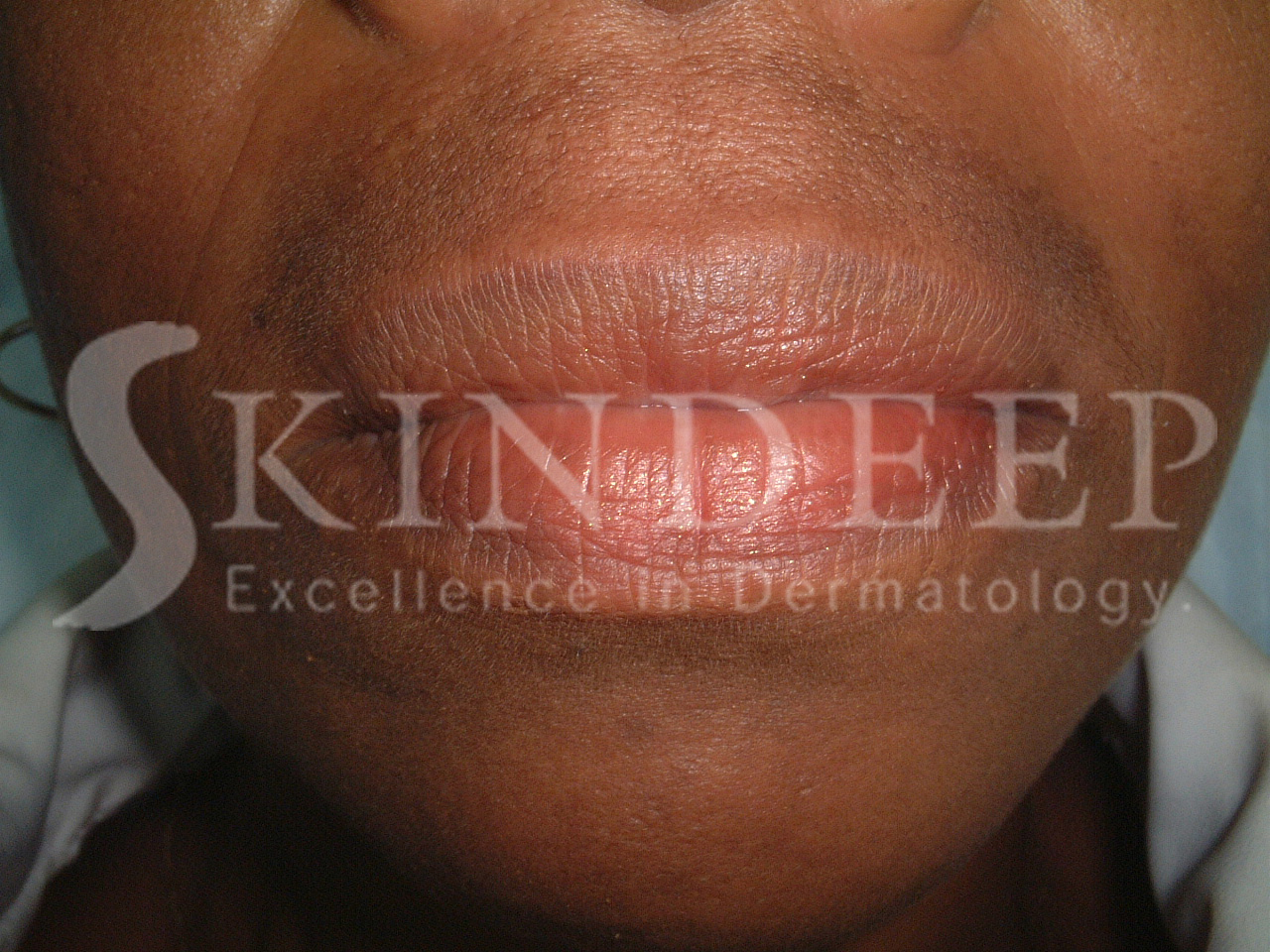
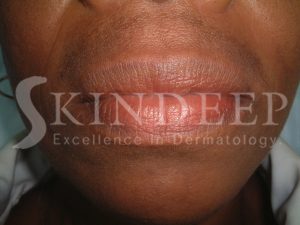
Melasma appears as dark brown macules or larger patches on the face. The common patterns are:
- Centrofacial pattern– forehead, cheeks, nose and above the upper lip.
- Malar pattern – the cheeks and nose
- Lateral cheek pattern
- Mandibular pattern – along the jawline
- Brachial pattern – shoulders and upper arms
Your Dermatologist usually makes the diagnosis of this condition easily by clinical examination. Very rarely is a biopsy required unless there is ambiguity related to the diagnosis. A woods lamp examination is used to determine the depth of the pigment and therefore possible response and duration of treatment.
General measures are important in the effective control of this condition. In temperate countries with four seasons it is a disorder of summer. In Barbados with sunlight all year round, it is important to practice sun protection with broad spectrum SPF 60 or above. Camouflage make up can also cover and physically protect the skin. Hormonal contraception should be discontinued where possible.
Lightening agents that work by inhibiting the tyrosinase enzyme are used to reduce pigment production. Azealic acid preparations are safe but can be associated with irritation and are available in lotions, gels and creams. Kojic acid soaps are widely available here and do a similar job of inhibiting melanin production. Hydroquinone should be used with caution and under medical supervision. It should not be used in concentrations greater than 4% and has to be applied accurately to avoid unwanted lightening of normal skin. The use of hydroquinone is banned in some parts of the world due to the possibility of paradoxical permanent darkening called ochronosis, which occurs with prolonged use of concentrations over 4%.
Superficial (epidermal) forms of melasma benefit from treatment with peeling agents such as Salicylic acid, topical retinoids, and alpha hydroxy acids e.g. Glycolic and lactic Acid. 70% Glycolic acid is frequently used in chemical peels by dermatlogists but usually a series of treatments are required. All peeling agents can cause irritation exhibited as redness or dryness and should to gradually introduced to any treatment regimen.
Combination topical therapy is most efficient as a single treatment option and variations of the Kligman’s formula, which consists of hydroquinone, tretinoin and a topical steroid, are often used.
Various forms of lasers and intense pulsed light (IPL) are the newest additions to the treatment armamentarium. Excessive lightening and darkening of the treatment areas are unwanted side effects in some cases. Experienced Dermatologists best perform these procedures. Darker skin types are more prone to adverse side effects.
Due to the recurrent nature of the condition, patients must appreciate the need for lifestyle change and maintenance for sustained clearance. Exposure to excessive sunlight over a period of weeks can reverse successful clearance of pigmentation. Cases associated with pregnancy usually resolve months after delivery.