Cutaneous larva migrans is a parasitic skin disease caused by the penetration of hookworm larvae into the skin. These hookworms usually live in the small intestines of dogs, cats and other animals and have a bend in their body close to the head giving them the appearance of a hook.
CLM is also called the “creeping eruption” and is most commonly caused by Ankylostoma braziliense. All ages, sexes and races in the tropical or subtropical areas are susceptible to this infestation. Sunbathing as well as sitting and walking on the beach barefooted are the main risk factors for infection. Faecal contamination in soil around houses and construction sites or playing in sandpits are common areas inhabited by larvae.
Infected animals deposit faeces containing hookworm eggs. These eggs hatch in moist, sandy soils forming larvae that penetrate human skin via the hair follicles, tiny cracks or even through intact skin. Migration under the skin begins after a few days or weeks. Humans are incidental dead end hosts as the larvae are unable to penetrate the basement membrane to enter the body.

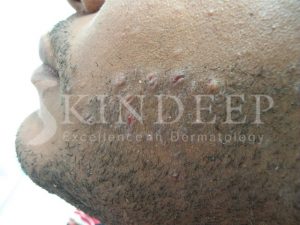
There may be a prickling or stinging sensation within 30 minutes of the larvae penetrating the skin. The hands, feet, knees, abdomen and buttocks are the most common sites of penetration. A 2-3 mm wide snake like (serpiginous) track forms and extends at the rate of 0.2 to 2 cm per day. These tracks are skin coloured or red and extremely itchy! Some unfortunate individuals can have several tracks with such severe itching that sleep can be affected. Intense scratching can lead to secondary bacterial infection.

Left untreated the infection can continue for up to four weeks until the larvae die. The most efficient treatment is oral albendazole for three consecutive days. Alternatively a paste can be made from crushed albendazole tablets or 10% thiabendazole applied for up to two weeks. Larvae can be physically killed by applying spraying liquid nitrogen on the distil end of the track. This freezing treatment can be uncomfortable and may have to be repeated. Antihistamines and topical steroid creams help to control itching while antibiotic creams treat secondary bacterial infection.
Localised itching in the presence of a spreading snake like eruption should always suggest this unique tropical disease.