This is an inflammatory condition of one or both of the lower extremities due to insufficiency of the leg veins. It is also known as stasis dermatitis and venous eczema.
Valves in the deep, perforator and superficial veins help blood to flow from the lower limbs to the heart efficiently. Incompetent valves allow flow in the opposite direction and this increases venous pressure, which results in fluid leaking into the surrounding tissues. This then triggers inflammation in the skin.

Gravitational eczema is more common in middle-aged patients with females being more commonly affected. Smoking, obesity, pregnancy and inactivity associated with excessive sitting or standing are aggravating factors. Acquired venous insufficiency due to surgery, trauma and deep vein thrombosis can precipitate this condition.

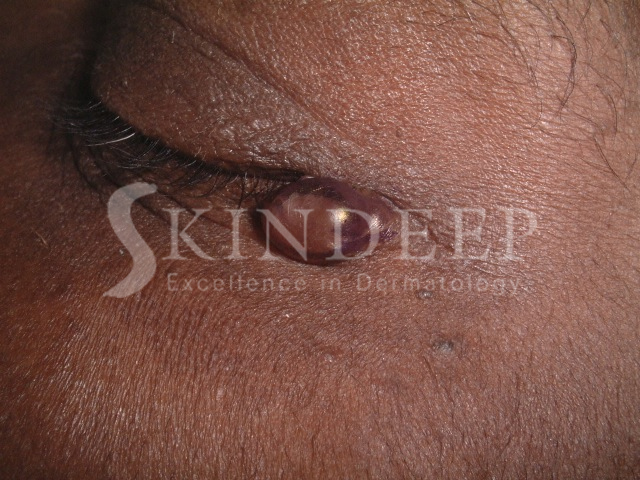
The earliest symptom is increasing swelling of the ankles during the day, which resolves with lying in bed while sleeping. This becomes more severe and constant and is associated with aching discomfort and varicose veins. A dark pigmentation then appears just above the ankle due to haemosiderin deposition in the tissues from the breakdown of red blood cells. Eczema changes range from itchy red papules and blisters (acute) to dark thickened, hard, cracked and peeling skin (chronic) either in patches or generally on the lower two thirds of the leg. Net like or poly angular atrophic white scars with red bumps are sometimes present, especially on the lower inner aspect of the ankle, and these are called atrophie blanche.
Lipodermatosclerosis is the name given to the chronic changes associated with chronic venous insufficiency. These changes consist of haemosiderin pigmentation, atrophie blanche and a hardening/thickening of the lower third of the legs due to inflammation of the subcutaneous fat. The leg takes on an “inverted champagne bottle” or rolling pin appearance that is permanent.
Complications of venous eczema include infection, which can take the form of a weeping honey coloured liquid associated with blisters and dark crusts called impetigo. Spreading superficial skin infection associated with warmth, redness and swelling is called cellulitis. Contact dermatitis can also occur due to the various medications and dressings used during treatment.
The most feared complication however is the venous ulcer that can be chronic and cause significant emotional distress as well as decreased quality of life.
It is important to keep physically active and to avoid standing for long periods without engaging the calf muscles as a pump to return blood to the heart. While sitting or lying down the legs should be elevated above the hips. The use of gentle soaps and moisturisers allows for proper surveillance and detection of complications. Compression bandages and hosiery are required to limit the swelling from vein incompetence. Above all, trauma must be avoided as it can precipitate ulceration.
Oral medications are used to improve vein circulation like pentoxifylline. Patients with a history of deep vein thrombosis are kept on oral prophylactic medication and generally infection is treated with topical or oral antibiotics. Wet eczemas and infections require wet compresses, with potassium permanganate or diluted white vinegar, and respond to steroid creams. Chronic eczematous changes respond better to greasy moisturisers and steroid ointments.
Ulcers are kept clean and dressed and in some cases physical methods like vacuum dressings or hyperbaric oxygen are used. Surgical methods are very effective including skin grafts, flap closure, laser ablation, endoscopic vein surgery and sclerotherapy to name a few.

In our country where obesity and diabetes is so common, stasis dermatitis and subsequent ulcer formation can contribute to loss of limb, disability and morbidity. Since it is largely preventable, we must all do our part via lifestyle changes including diet and exercise to reduce the burden of care on our health budget.
Early intervention by your doctor is critical to enable positive outcomes.