The kidneys play the important role of removing waste and excess fluids from the body. Common medical conditions like diabetes, hypertension, autoimmune disease, kidney infections and congenital polycystic kidneys contribute to chronic disease. Associated risk factors for disease include, smoking, obesity, high cholesterol, increasing age and family history.
A variety of skin changes are associated with chronic renal failure. In addition to the significant threat to health posed by kidney disease, skin changes often reduce the quality of life. These diseases may be manifestations of an underlying illness or due to uraemia, which literally means urine in the blood. We will concentrate on a few of these skin problems, which suggest poor kidney function.
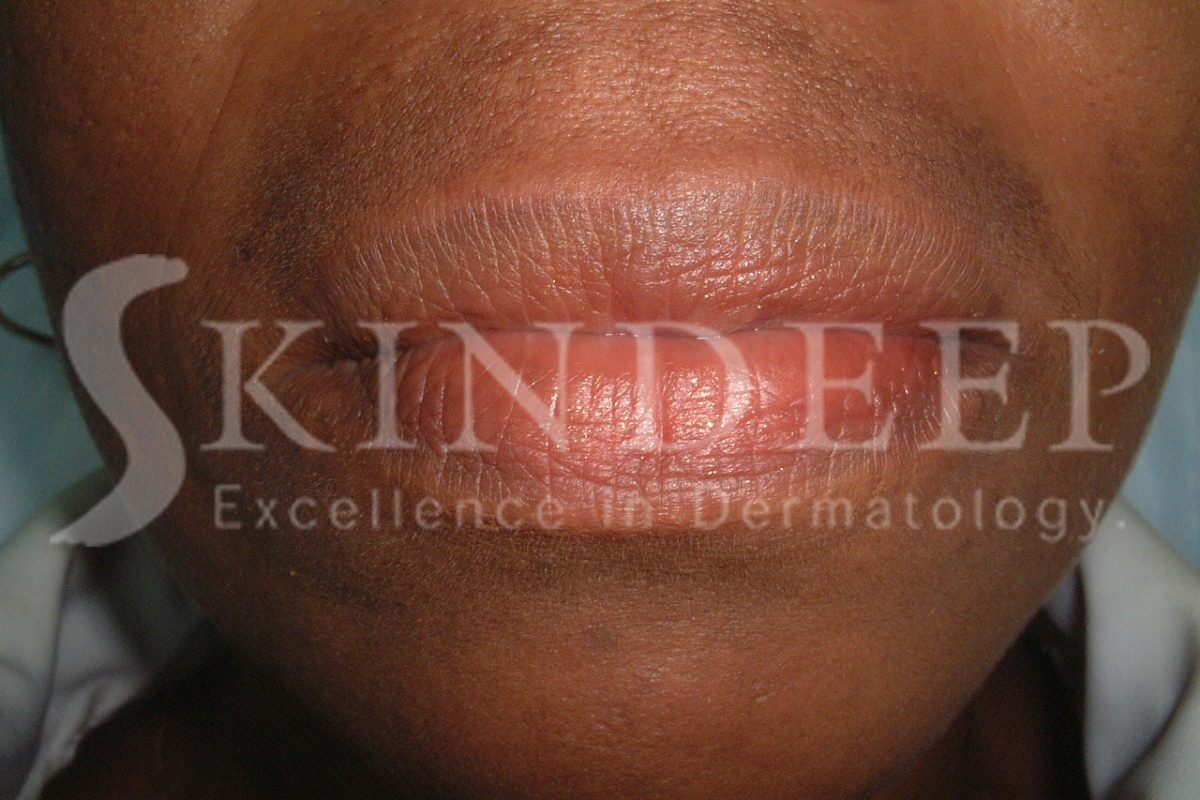
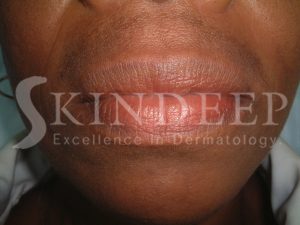
Anaemia due to low levels of red blood cells causes the (mucous membranes) lining of the eyes, mouth to appear pale. Uraemic stomatitis is an uncommon event resulting in a whitish thickening of the tongue and inner mouth, which can also result in ulcer formation. Dry mouth (Xerostomia), inflammation of the gums and angles of the mouth can also occur. The latter is called angular stomatitis.
Alteration in the general colour of the skin is a common association. A brown to slate grey generalised discoloration due to excessive haemosiderin deposition occurs as a consequence of iron overload from blood transfusions. Extensive darkening in the sun-exposed areas can be a possibility due to increasing hormone levels associated with melanocyte stimulation. It is important to avoid excessive sun exposure.
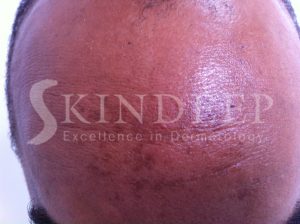
Generalised skin dryness (Xerosis) that is aggravated by cold weather or air conditioning is often present. Xerosis causes uncomfortable skin tightness and itching and can progress into other severe forms of dryness and thickening called icthiosis. Dry skin has excessive lines, cracks, lacks lustre and tends to be inelastic. It is best to use gentle cleansers and greasy moisturisers on a routine basis.
Pruritis (itching) is a very common problem faced by patients with renal failure and is called Uraemic Pruritis. Itching may be generalised or localised to the trunk, head arms or legs. These daily bouts of scratching tend to get worst at night and can prevent sleep. Dialysis reduces its severity significantly but unfortunately it may only take 48 hours to revert to maximum. In addition to dryness there may be numerous excoriations (scratch marks) with associated discoloration. Secondary bacterial infection is a complication of scratching which also has to be managed. Additional sequelae include eczema changes ranging from acute to chronic chronic as well as nodular prurigo. The latter refers to thickened dark nodules in itchy areas, which are very persistent. The severity of these symptoms can results in anxiety, depression, and agitation in over 50% of those affected.