Viral warts are caused by infections with the Human Papillomavirus. There are at least 70 subtypes of this virus. Warts can appear anywhere on the body and commonly affect children and young adults even though all age groups are susceptible. Warts do not have “roots” and they only grow in the upper layer of the skin called the epidermis.

This infection is spread by skin-to-skin contact between individuals, autoinoculation, or from objects and surfaces. Skin that is damaged or wet and macerated is more susceptible to infection. Biting and sucking your fingers can also predispose you to warts.
Communal bathing and changing facilities such as hotel rooms, bathrooms and swimming pools are areas where warts are contracted. Individuals with weakened immune systems or on some types of medication are also prone to chronic, stubborn episodes.
TYPES OF WARTS
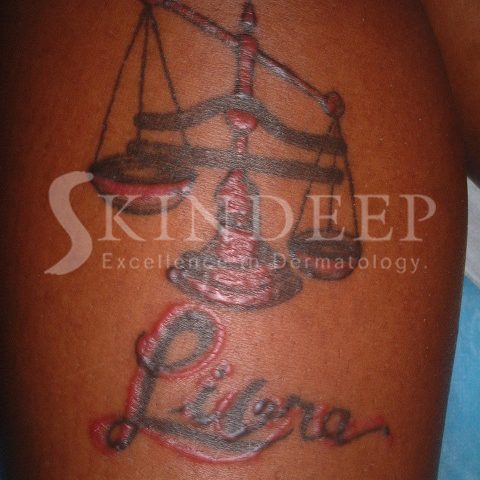
COMMON WARTS take the form of roughened skin coloured papules, which may be single or multiple. They are found most commonly on the dorsum of hands, toes, knees and elbows.
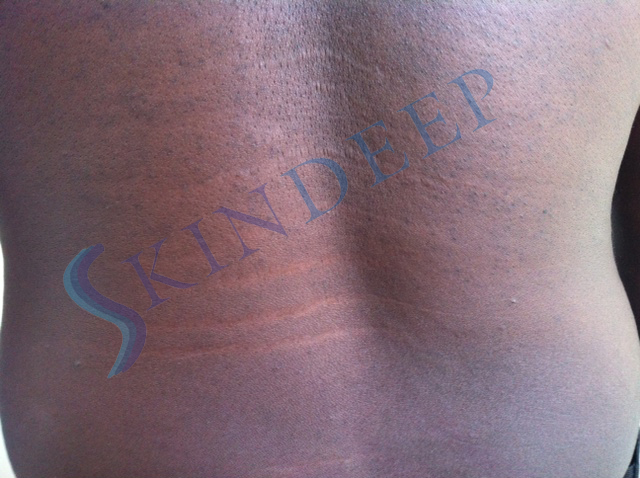
PLANTAR WARTS present as roughened flat areas, which penetrate deeply due to the pressure of your body weight and occur on the soles of the feet.
The MOSAIC pattern refers to clusters of warts over an area, which can be several centimetres wide. They can be painful and create difficulty with walking and are resistant to treatment.
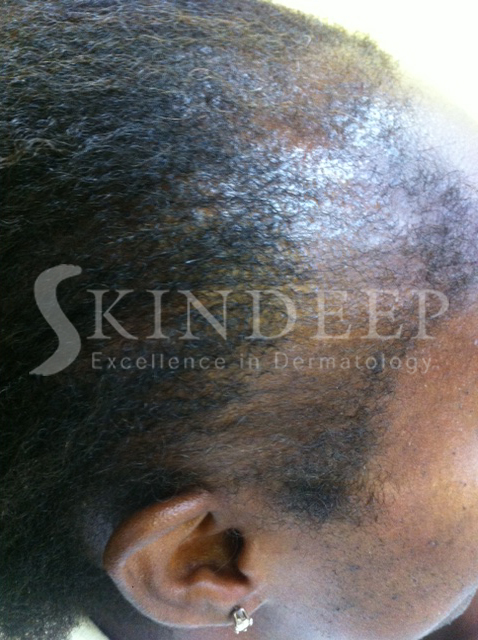
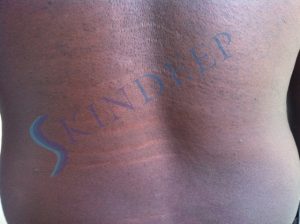
PLANE WARTS are usually 1-3 mm flat-topped papules that are smooth or have a slightly dry surface. The colour can vary from skin coloured to darker or lighter. The face and limbs are most often affected and they can be numerous. Shaving, incidental trauma and topical steroids spread them.
PERIUNGIAL WARTS occur around and under nails sometimes distorting nail growth. These warts can be stubborn as well.
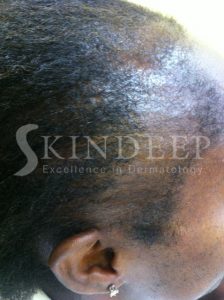
FILIFORM WARTS usually present as finger like growths on a stalk.
GENITAL WARTS appear in various clinical forms that are transmitted sexually and can predispose to cervical, vulval and penile cancer.
DIAGNOSIS
Warts are easy to diagnose clinically but there are some situations where corns, seborrhoeic keratoses or punctate keratodermas can cause confusion. Very often black dots are observed within a wart, which represent thrombosed blood vessels. Scraping or paring of a wart results in bleeding points, corresponding to these blood vessels. Scraping of a corn however, results in skin which looks progressively more normal. Corns are also painful to direct pressure.

TREATMENT
Left alone about 3 in ten warts disappear in ten weeks and even more resolve in 1-2 years.
There is a study that suggests covering common warts with adhesive/duct tape for six days a week, with the seventh used for soaking and paring down the exposed wart actually works. Results vary from encouraging to useless.
Salicylic acid wart paints can be used to treat warts in all areas except the face and genitals. It is best to soften the wart by soaking in warm soapy water, followed by paring with a pumice stone or emery board. The paint is applied accurately to the wart and then covered with plaster or duct tape. This process is repeated for approximately four months or until resolution.
Liquid nitrogen is applied to warts with a cotton bud or sprayed on to cause three or four freeze thawing cycles in one treatment. These treatments are performed every three to four weeks until the warts disappear. On average approximately one to four treatments are required but some stubborn warts require more. Aggressive freezing sessions can result in a blister that can be popped with a clean needle and treated with topical antibiotic. Over the counter spray freezing methods are less effective than liquid nitrogen. Combining freezing and cryotherapy is usually the best treatment.

In cases where a wart is stubborn and solitary (or just a few in number) a surgical approach can be used as a last resort. Unlike the other methods this results in a scar. The method most often used is curettage and electrosurgery in which the wart is scraped and scooped out with a curette before the wound is cauterised electrically. These wounds heal in about two weeks.
Lasers, cytotoxic drugs and immune modulators are also used to treat warts.
The spread of warts can be minimised by avoiding the sharing of towels, shoes as well as socks. When swimming, a waterproof plaster should be used to cover your wart. In the case of individuals with plantar warts, it is important to wear slippers in communal bathrooms and showers. Younger children should be discouraged from sucking fingers and biting nails if they already have warts.